Medicaid Long Term Care: A Safety Net for Older Adults
The Medicaid Long Term Care programs are a “safety net” for older adults who run out of money to pay for their long-term care needs in Washington State. This State and Federal program provides essential funds for housing and long-term care for vulnerable adults. Some assisted living facilities, memory care facilities, and adult family homes accept Medicaid as a payment source; however, many do not. If you are considering one that does accept Medicaid, it is important to review their Medicaid acceptance agreement carefully. I will call all facilities “homes” since that term sounds more inviting to me.
Navigating Medicaid Eligibility
For Medicaid eligibility, one must be assessed both medically and financially. Before considering a move into a home that accepts Medicaid, one needs to estimate how long it will take to “spend down” to meet Medicaid asset limitations. For an unmarried person, the total liquid asset limitation is $2,000 (almost nothing). In this case, to get a rough estimate of how many months it will take to spend down your assets, divide total assets by the estimated cost of monthly rent and care, less income, plus expenses. For example, a person with 200,000 in assets, paying 8,000 per month for rent and care, 400 for expenses, with 2000 per month in income, can pay privately for an estimated 31 months. For couples, this is much more complicated. Medical eligibility, based on help needed for activities of daily living and income eligibility, will not be discussed here.
The Private Pay Requirement
Most homes accepting Medicaid as a payment source require a “private pay” period. This means one must pay the private rate, including annual cost of living increases and increases due to the level of care, for a certain period before the home will accept Medicaid as a payment source. These private pay periods can range from zero to 5 years.
Limitations and Considerations
Some homes limit themselves in the number of “beds” or “rooms” allocated for Medicaid as a payment source. For example, an adult family home may limit the number of rooms for Medicaid to two. Understanding this part of the agreement in detail before moving in is critical. Some further questions include what happens when you are ready to convert to Medicaid and the Medicaid rooms are taken? What happens if the home drops its Medicaid “program” or is sold to a new owner?
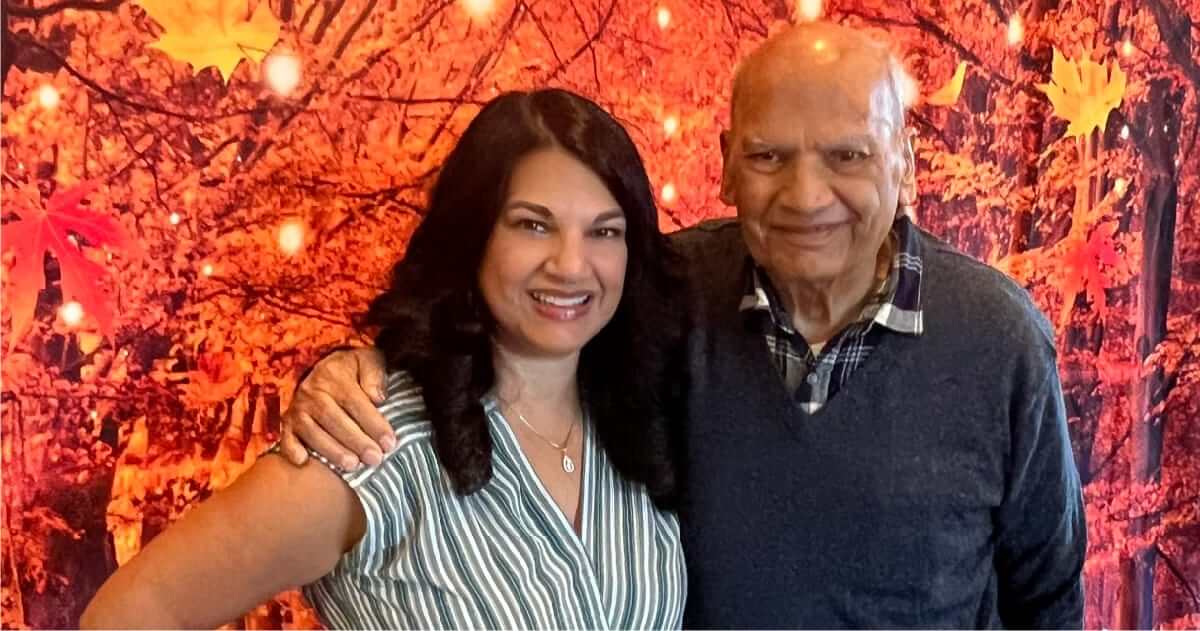
A Real-World Example
Patty, not her real name, is an example of a woman I served. She and her family consulted with an elder law attorney, and a spend-down period of 28 months was estimated. I found a lovely home that contracted for a minimum of 24 months of private pay, which satisfied her spend-down period. At about 26 months in, Patty was approved for Medicaid, enabling her to stay in the home with the same loving care providers and the residents she had befriended.
The Importance of Planning and Professional Guidance
Although conversion to Medicaid may be years away, it is important to plan for it carefully. The benefit of staying in the same home you know and love through the Medicaid Program is unquestionable. One of the services our clients find most valuable is our review of a home’s rental agreement, specifically regarding the home’s Medicaid acceptance policy. “No surprises and avoiding unnecessary moves” is a fundamental part of our placement service.
My disclaimer is that I am not an attorney or financial advisor and do not work for the Department of Social and Health Services. You are strongly encouraged to consult with each of these professionals and State Caseworkers regarding Medicaid eligibility and securing a home for long-term care.